Male infertility is associated with an increased risk of prostate cancer in a large cohort study.
A comprehensive cohort study on the association of ART (Assisted Reproduction Techniques) conducted in Sweden was reported in its entirety in the presenting in the UK British Journal of Medicine presented for the first time at the 2018 ESHRE Annual Meeting in Barcelona that involving more than 1.2 million parents links a significantly increased risk of prostate cancer to male fertility, in patients who underwent IVF and had to complete their ICSI treatment.
The study, which obtained data from three comprehensive Swedish registries to Identify all parents and their first child born in Sweden between 1994 and 2014, found that those who had had ART (and especially ICSI) to help conceive their children had a statistically significant higher risk of prostate cancer than controls (than those naturally conceived by their children). This overall risk in ICSI parents is mainly explained by prostate cancer diagnosed before age 55 with “early onset,” where the risk was nearly three times that of controls.
Although the authors themselves (as well as several commenters) cannot offer any biological explanation for the findings, they emphasize this, because ICSI is a reasonable marker of male infertility, especially in Sweden, where its indication remains exclusively for male cases … « The increased risk of prostate cancer is definitely not due to ICSI treatment per se, “said first author Yahia Al-Jebari of Lund University,” which we know has no biological impact on man. ”
In suggesting a possible explanation for the findings, a BMJ editorial accompanying the study and highlighting the link to male infertility rather than ICSI itself noted a genetic association between microdeletions on the Y chromosome (well established as a cause of severe male infertility ) and genes on the same chromosome that is known to be associated with prostate cancer. The editorial added that mutations in DNA repair genes and epigenetic and environmental modulators had also suggested a link between male infertility and prostate cancer.
Some, but not all, previous studies have found a link between male infertility and the risk of prostate cancer. A 2010 NIH study, for example, found that infertility can double a man’s risk of aggressive prostate cancer; Although the number of cases of prostate cancer among infertile and fertile men was no different, the nature of their cancers did.
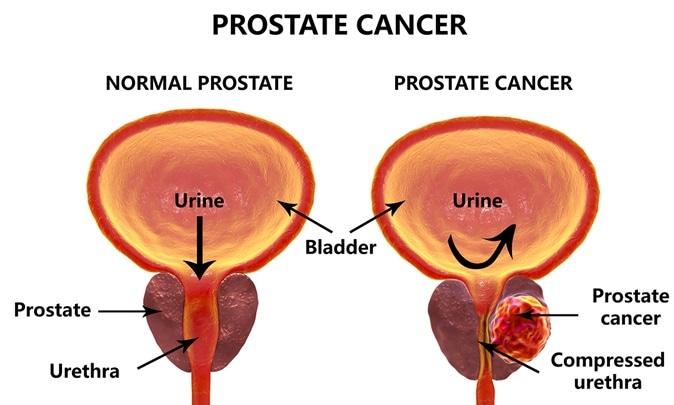
Fathers who used ICSI had a 60% higher risk and those who used IVF had a 30% higher risk than men who conceived naturally. And given the incidence of “early onset” disease in this study and its overall poor prognosis, they propose that men who have ART “may benefit from early detection.” According to the authors, prostate-specific antigen screening appears to be the most appropriate, most cost-effective, and least invasive first-line method of early detection. However, the accompanying editorial notes that “the assessment is controversial due to the lack of survival benefits and the harm of overdiagnosis and overtreatment that can follow a positive screening test.”
You still can’t do your spermatobioscopy? Or your prostate antigen don’t wait any longer and come to a specialized biology of human reproduction consultation.
Take care of your health and make an appointment with our specialist.
Al-Jebari Y, Elenkov A, Wirestrand E, et al. Prostate Cancer Risk for Men Who Are Fathers Through Assisted Reproduction: A National Population-Based Registry Study. BMJ 2019; 366: doi.org/10.1136/bmj.l5214.
Sharma A, Jayasena CN. Male infertility linked to the risk of prostate cancer. BMJ 2019; 366: doi: 10.1136 / bmj.l5525.
Walsh TJ, Schembri M, Turek PJ et al. Increased risk of high-grade prostate cancer among infertile men. Cancer 2010; 116: 2140-2147.
