Hypothyroidism It is a very common endocrinological disorder in the Reproductive Stage in both sexes, which results from deficiency of the Thyroid Hormone.
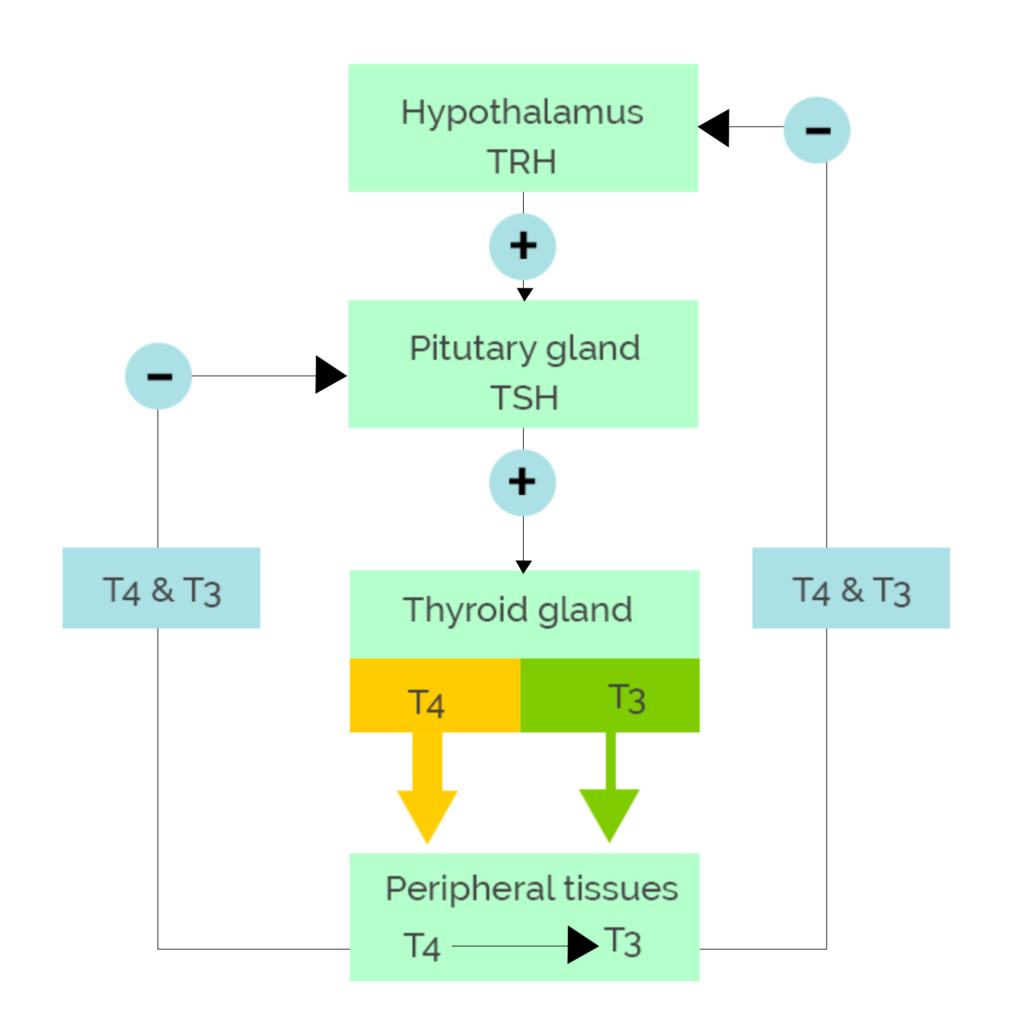
In the United States and other areas of Mexico, salt is supplemented with iodine or other components or foods to avoid increasing the risk of suffering from it, since worldwide iodine deficiency continues to be the main cause of this condition; But there are other diseases within the thyroid called Autoimmune (Hashimoto’s disease) which is the most common cause in hypothyroidism. This image below shows the hypothalamic-pituitary-thyroid axis. Circulating thyroid hormone levels are regulated by a complex feedback system that involves the hypothalamus and the pituitary gland.
Signs and symptoms
Hypothyroidism is commonly manifested by decreased physical and mental activity, but can be asymptomatic. The symptoms and signs are often subtle and not sensitive or specific.
The following are symptoms of hypothyroidism:
 Fatigue, loss of energy, lethargy.
Fatigue, loss of energy, lethargy.- Weight gain Decreased appetite
- Cold intolerance
- Dry Skin
- Hair loss
- Drowsiness
- Muscle pain, joint pain, weakness in the extremities.
- Depression
- Emotional lability, mental deterioration
- Forgetfulness, impaired memory, inability to concentrate
- Constipation
- Menstrual disorders, impaired fertility.
- Decreased perspiration
- Paresthesia and nerve entrapment syndromes
- Blurry vision
- Decreased hearing,
- Feeling of fullness in the throat.
The following are symptoms of Hashimoto Hypothyroidism
- Painless thyroid enlargement
- Exhaustion
- Transient neck pain, sore throat, or both
Physical signs of hypothyroidism include the following:
- Weight gain
- Decreased speech and movement.
- Dry Skin
- Jaundice
- Pallor
- Thick, brittle, straw-looking hair
- Hair loss from scalp, underarm hair, pubic hair, or a combination
- Dull facial expression
- Thick facial features
- Periorbital swelling
- Macroglossia
- Goiter (simple or nodular)
- Hoarseness
- Decreased systolic blood pressure and increased diastolic blood pressure
- Bradycardia
- Pericardial effusion
- Abdominal bloating, ascites (rare)
- Hypothermia (only in severe hypothyroid states)
- Non-stabbing edema (myxedema)
- Pitting edema of the lower extremities
- Hyporeflexia with delayed relaxation, ataxia, or both
Myxedema coma is a severe form of hypothyroidism that occurs most frequently in people with undiagnosed or untreated hypothyroidism who are under external stress. The characteristics are the following:
- Altered mental state
- Hypothermia
- Bradycardia
- Hypercarbia
- Hyponatremia
There may be cardiomegaly, pericardial effusion, cardiogenic shock, and ascites.
 Diagnosis
Diagnosis
Third-generation thyroid-stimulating hormone (TSH) assays are generally the most sensitive screening tool for primary hypothyroidism. If TSH levels are above the reference range, the next step is to measure free thyroxine (T4) or free thyroxine index (FTI), which serves as a substitute for free hormone level. Routine measurement of triiodothyronine (T3) is not recommended.
Biotin, a popular health supplement, can interfere with immunoassays for many hormones, resulting in falsely elevated or suppressed values, including thyroid levels. To avoid misleading test results, the American Thyroid Association recommends stopping biotin consumption at least 2 days before your thyroid test.
Abnormalities in complete blood count and metabolic profile that can be found in patients with hypothyroidism include the following:
- Anemia
- Dilutional hyponatremia
- Hyperlipidemia
- Reversible creatinine increases
- Elevations in transaminases and creatinine kinase
There are no universal screening recommendations for thyroid disease in adults. The American Thyroid Association recommends screening at age 35 and thereafter every 5 years, paying more attention to high-risk patients, such as the following [4]:
 Treatment:
Treatment:
Levothyroxine monotherapy (LT4) remains the treatment of choice for hypothyroidism.
Clinical benefits begin in 3-5 days and stabilize after 4-6 weeks.
Reaching a TSH level within the reference range can take several months. LT4 dose changes should be made every 6-8 weeks until the patient’s TSH is within the target range.
After dose stabilization, patients can be monitored with annual clinical evaluations and TSH monitoring.
Patients should be monitored for symptoms and signs of overtreatment, including the following:
- Tachycardia
- Palpitations
- Atrial fibrillation
- Nervousness
- Fatigue
- Headache
- Increased excitability
- Insomnia
- Tremors
In patients who continue to have symptoms despite normalization of their TSH level, other causes than hypothyroidism should be considered. In some cases, however, persistence of symptoms results from altered conversion of T4 to T3 in the brain; These patients may benefit from LT4 / liothyronine (LT3) combination therapy.
Onset or discontinuation of estrogen and androgens should be followed by reassessment of steady-state serum TSH, since these medications may alter the requirement of levothyroxine.
Monitoring of serum TSH is advisable when starting medications such as phenobarbital, phenytoin, carbamazepine, rifampin and sertraline.
When deciding on an initial dose of levothyroxine, the patient’s weight, lean body mass, state of pregnancy, etiology of hypothyroidism, degree of TSH elevation, age, and general clinical context should be considered, including the presence of heart disease. The appropriate serum TSH goal should also be considered for the clinical situation.
Thyroid hormone therapy should be started as an initial complete replacement or as a partial replacement with gradual increases in the titrated dose upwards using serum TSH as a target.
Dose adjustments should be made in the face of significant changes in body weight, with aging and with pregnancy; TSH assessment should be performed 4 to 6 weeks after any dose change.
The reference ranges for serum TSH levels are higher in older populations (eg,> 65 years), so higher serum TSH targets may be appropriate.
 more information, consult your Human Reproduction Biologist or endocrinologist to give you the ideal treatment since Fertility affects your reproductive prognosis, since it may be the first cause of repeat Abortions, among others .
more information, consult your Human Reproduction Biologist or endocrinologist to give you the ideal treatment since Fertility affects your reproductive prognosis, since it may be the first cause of repeat Abortions, among others .
