
The term in vitro fertilization, or IVF, literally means fertilization “in glass” and refers to the process in which a woman’s eggs are fertilized outside her body in the laboratory. The resulting embryos are transferred back to the uterus a few days later.
Under the care of a specialized physician, the woman receives fertility drugs to stimulate her ovaries to produce many follicles. Follicles are the small fluid-filled structures that develop in the ovaries, each of which will hopefully contain an egg. The number and size of the developing follicles is measured by transvaginal ultrasound. The exact number of follicles that develop varies between patients. The final preparation for egg retrieval involves an injection of hormones that mimics the natural trigger for ovulation. Egg retrieval will take place 36-38 hours after this injection.
High specialty operating room at IREGA
Egg retrieval is a medical procedure that is carried out in the clinic under local anesthesia. The transvaginal ultrasound probe is used to visualize the ovaries and a needle attached to the probe is passed through the vaginal wall into the follicles. The fluid within each follicle is aspirated and instantly examined in the laboratory for the presence of an egg. After identification, the eggs are washed and transferred to a special culture medium in Petri dishes in an incubator.
The male patient provides a semen sample and, in the laboratory, a concentrated preparation of the best motile sperm is extracted from the semen sample. This sperm preparation is added to the plates containing the eggs, and they are incubated together overnight, this is what is known as conventional IVF.

Some couples require an alternative form of insemination called ISCI, which involves injecting a single sperm into each egg with a very fine needle, rather than mixing the eggs and sperm in a plate. Intracytoplasmic sperm injection (ICSI) is very similar to conventional IVF in the way that eggs and sperm are obtained from each partner. The difference between the two procedures is the method of achieving fertilization.
ICSI is performed in the laboratory by experienced embryologists using specialized equipment. Very few sperm are required and the ability of the sperm to penetrate the egg is no longer important as this has been assisted by the ICSI technique although it does not guarantee that fertilization will occur as the normal cellular events of fertilization must still occur Once the sperm has been placed in the egg, so that the way to fertilize the eggs, whether it is conventional IVF or ICSI, will depend on the characteristics of the sperm on the day of the procedure and not on whether any of these fertilization alternatives are more efficient than the other. 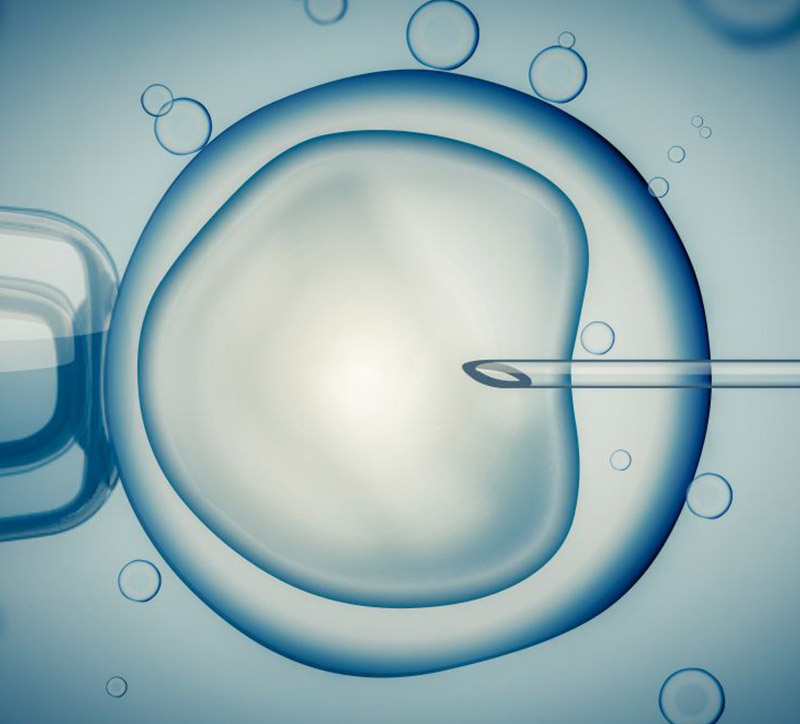
From the patient’s perspective, undergoing an ICSI treatment cycle is exactly the same as a conventional IVF cycle, and the same steps are involved, however circumstances in which ICSI may be appropriate include:
- When the sperm count is very low
- When sperm cannot move properly or are abnormal in other ways
- When sperm have been surgically retrieved from the epididymis (MESA / PESA) or testes (TESE / TESA), from urine or after electro-ejaculation
- When there are high levels of antibodies in the semen
- When there has been a previous fertilization failure using conventional IVF.
Finally and regardless of the insemination method used, in the morning after the eggs are retrieved, they are examined to see which ones have been fertilized. Fertilized eggs (zygotes) are routinely cultured in the laboratory until such time as the best embryos are selected and transferred back to the woman’s uterus.

Biol. Emanuel Mejía Jiménez
Jefe del Servicio de Laboratorio de Reproducción
